Are All White Patches on the Face a Sign of Vitiligo? Differential Diagnosis and Clinical Insights

Are All White Patches on the Face a Sign of Vitiligo? Differential Diagnosis and Clinical Insights
- 23 July 2025
- 197
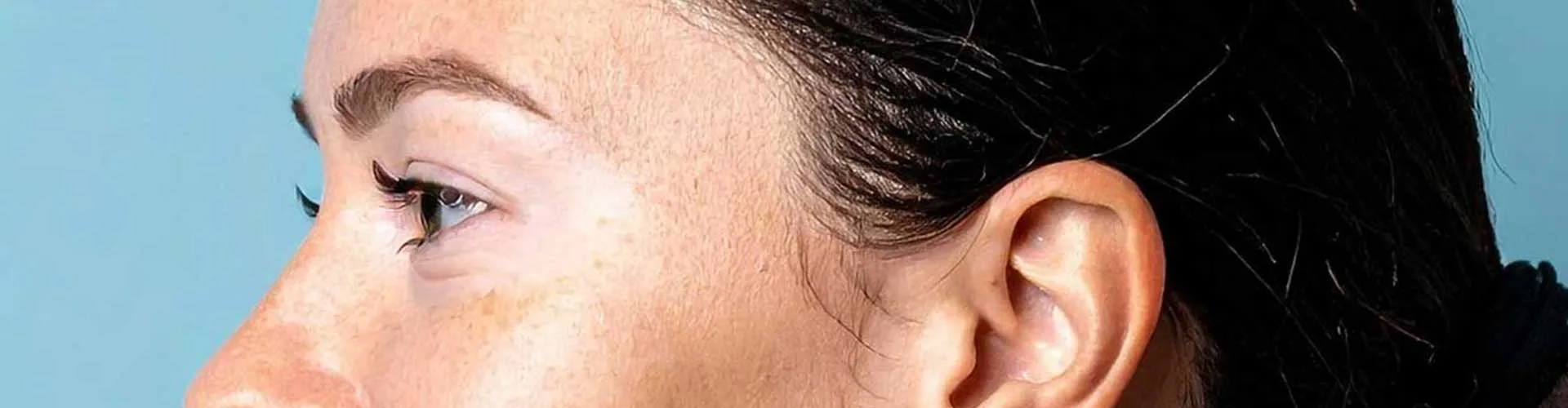
White patches on the face are a common dermatological concern that often leads people to suspect vitiligo. While vitiligo is one of the most recognized causes of depigmentation, not all white spots are vitiligo. In fact, there are numerous other skin conditions that present with similar features, including mild scaling, pigmentation loss, or inflammation.
Self-diagnosis can lead to unnecessary anxiety, delayed treatment, or inappropriate management. This comprehensive article aims to clarify the clinical presentation of vitiligo, highlight common differential diagnoses, and explore how dermatologists distinguish between various hypopigmented disorders of the face.
What Does Facial Vitiligo Typically Look Like?
Vitiligo is an autoimmune skin disorder that results in loss of melanocytes, the cells responsible for producing melanin. Facial vitiligo has a few characteristic features:
- Sharply demarcated, milky-white patches
- Commonly involves perioral (around the mouth), periorbital (around the eyes), and nasal regions
- Often symmetrical in distribution
- Usually non-scaly and not itchy
- May be associated with poliosis (white hair in the affected area)
- Lesions may enlarge slowly over time
However, the skin can also lose pigment for many other reasons, not necessarily related to vitiligo.
Conditions That Mimic Vitiligo on the Face
Many skin disorders can cause hypopigmentation or depigmentation, particularly in the facial region. The following conditions are frequently confused with vitiligo:
|
Condition |
Description |
Differentiating Features |
|
Pityriasis Alba |
Common in children; light patches with fine scaling |
Ill-defined borders, mild itch, seasonal flare-ups |
|
Tinea Versicolor |
Fungal infection by Malassezia species |
Fine scaling, trunk involvement, positive KOH test |
|
Post-Inflammatory Hypopigmentation (PIH) |
Follows eczema, burns, or injury |
History of prior skin inflammation |
|
Idiopathic Guttate Hypomelanosis |
Small round white macules in elderly |
Sun-exposed limbs; not the face usually |
|
Chemical Leukoderma |
Caused by contact with certain chemicals (e.g., phenols) |
History of exposure to skin irritants |
|
Lichen Sclerosus |
Rarely affects the face; causes white, atrophic plaques |
More common in genital regions |
|
Early Leprosy (Hansen’s disease) |
Endemic regions; white patches with sensory loss |
Numbness, nerve thickening, biopsy required |
Pityriasis Alba vs. Vitiligo
Among the differential diagnoses, pityriasis alba is the most commonly confused with vitiligo, especially in children. Key differences include:
- Mild scaling and roughness to touch
- Poorly defined borders
- May show mild redness before fading
- Common in atopic children
- Lesions typically resolve over time, often without treatment
- Appear more pronounced during summer due to tanning contrast
Unlike vitiligo, pityriasis alba is not an autoimmune condition and does not involve melanocyte destruction.
Diagnostic Tools and Dermatological Evaluation
To determine the exact cause of facial white patches, dermatologists use various tools and assessments:
- Wood’s Lamp Examination – Vitiligo lesions fluoresce bright white under UV light
- Clinical History – Onset, location, previous skin conditions, exposures
- KOH Test – Used to detect fungal elements in tinea versicolor
- Skin Biopsy – In uncertain cases, histopathological examination is needed
- Dermoscopy – Helps evaluate pigmentation patterns and vascular features
- Sensory Testing – Important if leprosy is a differential diagnosis
Accurate diagnosis is crucial for appropriate treatment and psychological reassurance.
Potentially Serious but Rare Conditions
Though uncommon, a few serious conditions may initially present with facial depigmentation:
- Hypopigmented Cutaneous Lupus – Associated with erythema, photosensitivity, systemic symptoms
- Leprosy (Hansen’s Disease) – Rare in most regions but still endemic in some; requires immediate attention
- Hypopigmented Melanoma – Exceptionally rare but should not be missed in atypical or changing lesions
Therefore, if the white patch is asymmetrical, enlarging, causing sensory changes, or has irregular borders, medical evaluation is urgent.
Treatment Based on Diagnosis
Management depends entirely on the underlying cause:
- Vitiligo: Topical corticosteroids, calcineurin inhibitors, phototherapy, laser treatment
- Pityriasis Alba: Moisturizers, gentle skin care, low-dose topical steroids if needed
- Tinea Versicolor: Antifungal creams or shampoos (e.g., ketoconazole, selenium sulfide)
- PIH: No specific treatment; addressing the original inflammation helps
- Chemical Leukoderma: Discontinue offending chemical; possible repigmentation with topical therapy
- Lichen Sclerosus: Topical corticosteroids or immunomodulators
- Leprosy: Multidrug antibiotic therapy under specialist supervision
Incorrect treatment may worsen symptoms or cause new complications, especially if vitiligo treatments are applied to fungal or infectious lesions.
Frequently Asked Questions
No. Many benign conditions like pityriasis alba or fungal infections can mimic vitiligo. A proper diagnosis is essential.
Yes. Tinea versicolor, in particular, can cause pale patches that resemble vitiligo but usually involve scaling and respond to antifungal treatment.
Typically no. Most vitiligo lesions are asymptomatic. If there is itching, another diagnosis should be considered.
Not always. Wood’s lamp and clinical features are often sufficient. A biopsy is only done in atypical or unclear cases.
Through visual inspection, Wood’s lamp, KOH testing, history, and sometimes dermoscopy or biopsy.